Published online Dec 26, 2018. doi: 10.12998/wjcc.v6.i16.1094
Peer-review started: August 23, 2018
First decision: October 5, 2018
Revised: October 16, 2018
Accepted: November 23, 2018
Article in press: November 24, 2018
Published online: December 26, 2018
Processing time: 123 Days and 11 Hours
To investigate safety and oncological feasibility of laparoscopic total gastrectomy (LTG) in overweight (OW) patients.
Patients who underwent total gastrectomy (110 laparoscopic, 211 open) for gastric cancer between January 1999 and July 2016 were included. Propensity score matching selected 152 patients (76 laparoscopic, 76 open), which were subsequently divided into the OW (≥ 25) or non-OW (< 25) group by body mass index. Postoperative outcomes of laparoscopic versus open approaches were compared between OW and non-OW groups.
In the propensity-matched population, baseline characteristics were comparable between the OW and non-OW groups for the laparoscopy and open groups. In the laparoscopy group, operative time was longer (P = 0.01) in the OW group, however, other perioperative results including complication rates were comparable between the non-OW and OW groups. In the open group, number of retrieved lymph nodes were less (P = 0.03) and local complication rate was more frequent (P = 0.03) in the OW group.
LTG in OW patients remains technically challenging but can be performed safely. Our findings imply that OW has a lesser effect on the laparoscopic versus open approach to total gastrectomy.
Core tip: The feasibility and safety of the laparoscopic approach in overweight (OW) patients and cases of total gastrectomy were already reported, but an assessment of the feasibility and safety of laparoscopic total gastrectomy (LTG) in OW patients has not yet been conducted. In the article we performed two main analyses. One is a comparison of postoperative outcomes after LTG between OW and non-OW patients. The other is that after open total gastrectomy. In order to balance the baseline characteristics between laparoscopy and open groups, we performed propensity score matching. We found out two main results through the analyses. One is LTG in OW patients is feasible and safe although it remains technically challenging (longer operation time). The other is OW has less impact on laparoscopic versus open approach.
- Citation: Nakagawa M, Kojima K, Inokuchi M, Kobayashi K, Tanioka T, Okuno K, Gokita K. Feasibility of laparoscopic total gastrectomy in overweight patients: Implications of less impact of overweight on laparoscopic versus open approach. World J Clin Cases 2018; 6(16): 1094-1100
- URL: https://www.wjgnet.com/2307-8960/full/v6/i16/1094.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i16.1094
Over the past few decades, the proportion of proximal gastric cancer among all gastric cancer cases has been increasing[1,2]. The standard treatment for proximal gastric cancer is total gastrectomy with adequate lymph node dissection, while the laparoscopic approach is also applied in some high-volume institutions[3,4]. Meanwhile, overweight (OW) is an important health issue worldwide, and the number of OW patients in Japan is also increasing[5]. Consequently, the number of laparoscopic total gastrectomy (LTG) procedures performed in OW patients is increasing.
OW is a risk factor for postoperative complications in gastrectomy because of the narrow and deep operative field, increased risk of friable tissues, and increased frequency of comorbidities[6,7]. While some previous studies reported on the feasibility of laparoscopic gastrectomy in OW patients, other articles showed that OW has a negative impact on laparoscopic gastrectomy, and this approach in OW patients remains technically challenging[8-11]. Total gastrectomy is also a demanding laparoscopic procedure in any case. Due to the difficulty of lymph node dissection and reconstruction, LTG procedures have yet to be standardized. Total gastrectomy and OW seems among the worst combinations for the laparoscopic approach. However, whether OW really has a worse impact on LTG compared to open total gastrectomy (OTG) remains unknown. Thus, in the present study, we focused on the differences in LTG postoperative outcomes between OW and non-OW patients. We also analyzed these results in the OTG group to evaluate the impact of OW on LTG versus OTG.
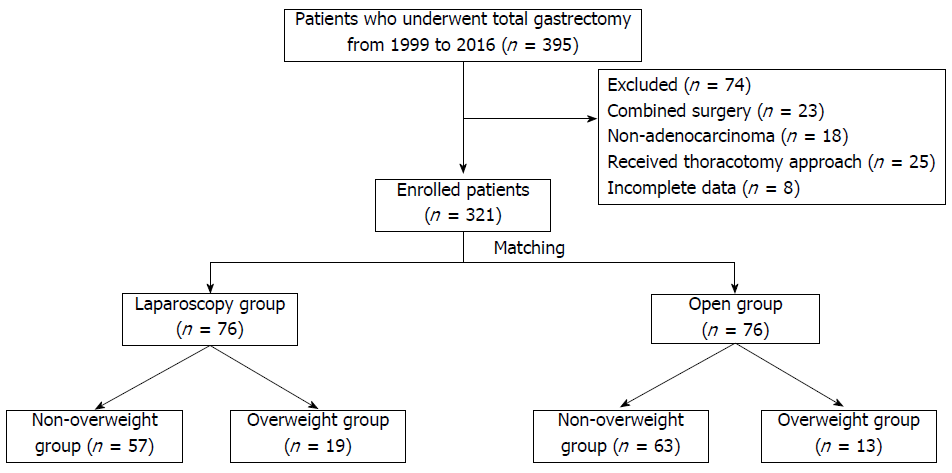
Between January 1999 and July 2016, 395 patients underwent total gastrectomy in the Department of Gastric Surgery, Tokyo Medical and Dental University Hospital, Tokyo, Japan. Patients with non-adenocarcinoma (n = 18), with combined surgery (n = 23), who received thoracotomy approach (n = 25), or for whom incomplete data were available (n = 8), were excluded; ultimately, 321 patients were enrolled in the present study. The following information was collected for each patient: age, sex, body mass index (BMI), operation period (early: 1999-2008, late: 2009-2016), pStage, tumor size, extent of lymph node dissection, presence or absence of splenectomy, operative time, intraoperative blood loss, number of retrieved lymph nodes, morbidity rate, and length of postoperative hospital stay.
The following variables were selected for propensity score matching: gender, age, operation period, extent of lymph node dissection, splenectomy, pT and, pN. The score was estimated using a logistic regression model and propensity-score-matched pairs without replacement (1:1 match with a caliper of width 0.1 standard deviations) were created.
After matching, both LTG and OTG group consisted of 76 patients for the analyses. Both groups were then divided into non-OW and OW groups (Figure 1). BMI was used to define OW. Patients with a BMI ≥ 25 were classified into the OW group, while those with a BMI < 25 were classified into the non-OW group.
Stages were classified according to the 7th edition of the Union for International Cancer Control classification system. Lymph node dissection was performed according to the guidelines of Japanese Gastric Cancer Association at the time of surgery[12,13]. In principle, the LTG approach was applied only in clinical Stage I patients. If clinical Stage II or III patients wished to undergo LTG, we performed it after offering a sufficient explanation and obtaining informed consent from the patients and their family members. A laparoscopic splenectomy was not performed unless the tumor was located at the greater curvature. In the LTG and OTG groups, Roux-en-Y reconstruction using a circular stapler was performed in all patients. In LTG, a laparoscopy-specific purse-string suturing device (END-PSD) was used to perform purse-string suturing and subsequent anvil insertion into the esophagus[14].
Complications were graded according to Clavien-Dindo classification[15]. All complications Grade I-V were counted complications, while those Grade IIIa or higher were considered severe complications.
Categorical values were analyzed using the chi-squared or Fischer’s exact analysis. Continuous values are shown as median and ranges. Normally distributed data were analyzed using independent t-tests, while non-normally distributed data were analyzed using the Mann-Whitney test. Overall survival (OS) was defined as the interval from surgery to death of any cause. Kaplan-Meier curves were used to compare prognoses between the non-OW and OW groups within the LTG and OTG groups. P values < 0.05 were considered statistically significant for all analyses. Statistical analyses were performed using SPSS version 19.0 software (IBM SPSS, Chicago, IL, United States).
Baseline characteristics are shown in Table 1. Before matching, in the OTG group versus the LTG group, more operations were performed in early period, D2 lymph node dissection and splenectomy were performed more frequently, mean tumor size was larger, tumor depth and lymph node classification were higher, and pStage were more advanced. After matching, baseline characteristics were comparable between both groups.
| All patients | Matched patients | ||||||
| LTG (n = 110) | OTG (n = 211) | P -values | LTG (n = 76) | OTG (n = 76) | P-values | ||
| Gender | Male | 81 | 162 | 0.53 | 55 | 62 | 0.18 |
| Female | 29 | 78 | 21 | 14 | |||
| Age (median, range) | 70 (32-83) | 69 (17-86) | 0.92 | 70 (32-83) | 71 (17-86) | 0.53 | |
| BMI (kg/m2) (median, range) | 23.2 (15.8-31.0) | 22.2 (13.6-38.3) | 0.07 | 21.9 (15.8-30.4) | 27.4 (13.6-35.4) | 0.35 | |
| period | Early | 39 | 148 | < 0.01 | 39 | 28 | 0.07 |
| Late | 71 | 63 | 37 | 48 | |||
| Extent of lymph node dissection | D2 < | 91 | 120 | < 0.01 | 57 | 53 | 0.47 |
| D2 | 22 | 142 | 19 | 23 | |||
| Splenectomy | Yes | 14 | 99 | < 0.01 | 14 | 19 | 0.33 |
| No | 96 | 112 | 62 | 57 | |||
| Tumor size (mm) (median, range) | 45 (6-200) | 70 (13-230) | < 0.01 | 52 (6-200) | 59 (14-213) | 0.14 | |
| pT | M | 21 | 7 | < 0.01 | 9 | 6 | 0.49 |
| SM | 34 | 23 | 21 | 17 | |||
| MP | 19 | 15 | 11 | 8 | |||
| SS | 20 | 71 | 19 | 20 | |||
| SE | 16 | 89 | 16 | 22 | |||
| SI | 0 | 5 | 0 | 2 | |||
| pN | N0 | 65 | 63 | < 0.01 | 38 | 36 | 0.38 |
| N1 | 19 | 30 | 13 | 7 | |||
| N2 | 13 | 40 | 12 | 12 | |||
| N3a | 9 | 48 | 9 | 12 | |||
| N3b | 4 | 30 | 4 | 9 | |||
| pStage | I | 66 | 37 | < 0.01 | 35 | 32 | 0.20 |
| II | 20 | 51 | 17 | 9 | |||
| III | 19 | 93 | 19 | 27 | |||
| IV | 5 | 30 | 5 | 8 | |||
A comparison of the baseline characteristics of non-OW and OW patients in the LTG and OTG groups is shown in Table 2. Aside from the statistical difference in BMI in the LTG and OTG groups, all variables such as gender, age, extent of lymph node dissection, splenectomy, tumor size, tumor depth, lymph node classification, and pStage were comparable between non-OW and OW patients in the LTG and OTG groups.
| LTG (n = 76) | OTG (n = 76) | ||||||
| non-OW (n = 57) | OW (n = 19) | P -values | non-OW (n = 63) | OW (n = 13) | P-values | ||
| Gender | Male | 42 | 13 | 0.66 | 52 | 10 | 0.45 |
| Female | 15 | 6 | 11 | 3 | |||
| Age (median, range) | 70 (40-83) | 64 (32-79) | 0.06 | 72 (17-80.6) | 71 (29-79) | 0.73 | |
| BMI (median, range) | 21.2 (15.8-24.8) | 26.6 (25.2-30.4) | < 0.01 | 20.9 (13.6-24.9) | 27.6 (25.0-35.4) | < 0.01 | |
| Extent of lymph node dissection | < D2 | 42 | 15 | 0.42 | 42 | 11 | 0.17 |
| D2 ≤ | 15 | 4 | 21 | 2 | |||
| Splenectomy | Yes | 11 | 3 | 0.73 | 17 | 2 | 0.31 |
| No | 46 | 16 | 46 | 11 | |||
| Tumor size (mm) (median, range) | 56 (6-185) | 50 (7-200) | 0.43 | 53 (14-211) | 75 (25-210) | 0.25 | |
| Depth of tumor | M | 7 | 2 | 0.11 | 6 | 0 | 0.37 |
| SM | 15 | 6 | 12 | 5 | |||
| MP | 5 | 6 | 7 | 1 | |||
| SS | 16 | 3 | 18 | 2 | |||
| SE | 14 | 2 | 18 | 4 | |||
| SI | 0 | 0 | 1 | 1 | |||
| Lymph node classification | N0 | 26 | 12 | 0.43 | 30 | 6 | 0.85 |
| N1 | 9 | 4 | 6 | 1 | |||
| N2 | 10 | 2 | 9 | 3 | |||
| N3a | 8 | 1 | 11 | 1 | |||
| N3b | 4 | 0 | 7 | 2 | |||
| pStage | I | 25 | 10 | 0.34 | 26 | 6 | 0.51 |
| II | 11 | 6 | 9 | 0 | |||
| III | 17 | 2 | 22 | 5 | |||
| IV | 4 | 1 | 6 | 2 | |||
The non-OW and OW patients’ perioperative results were compared in the LTG and OTG groups (Table 3). In the LTG group, although operative time was longer (P < 0.01), overall, local, and systemic complication rates were comparable between non-OW and OW patients (P = 0.49, 0.14, and 0.56, respectively).
| LTG (n = 76) | OTG (n = 76) | ||||||
| non-OW(n = 57) | OW(n = 19) | P-values | non-OW(n = 63) | OW(n = 13) | P -values | ||
| Operative time (min) (median, range) | 332 (209-541) | 400 (230-520) | 0.01 | 265 (134-810) | 276 (195-460) | 0.32 | |
| Estimated intraoperative blood loss (mL) (median, range) | 188 (0-2492) | 202 (0-1714) | 0.63 | 445 (90-3406) | 780 (104-1980) | 0.14 | |
| No. of retrieved lymph nodes (median, range) | 43 (8-71) | 36 (14-117) | 0.4 | 41 (9-89) | 29 (2-49) | 0.03 | |
| Morbidity (%) | Overall | 13 (23) | 5 (26) | 0.49 | 23 (37) | 8 (62) | 0.1 |
| Local | 7 (12) | 5 (26) | 0.14 | 14 (22) | 7 (54) | 0.03 | |
| Systemic | 8 (14) | 3 (16) | 0.56 | 13 (21) | 4 (31) | 0.32 | |
| Severe | 5 (9) | 3 (11) | 0.56 | 8 (13) | 4 (31) | 0.12 | |
| Anastomotic Leakage | 3 (5) | 3 (16) | 0.16 | 2 (3) | 3 (23) | 0.03 | |
| Anastomotic stricture | 1 (2) | 1 (5) | 0.44 | 1 (2) | 1 (8) | 0.32 | |
| Pancreatic fistula | 3 (5) | 0 (0) | 0.42 | 3 (5) | 2 (15) | 0.2 | |
| Abdominal abscess | 2 (4) | 0 (0) | 0.56 | 3 (5) | 2 (15) | 0.2 | |
| pulmonary | 5 (9) | 2 (11) | 0.90 | 9 (14) | 1 (8) | 0.46 | |
| Wound infection | 1 (2) | 1 (5) | 0.44 | 3 (5) | 2 (15) | 0.2 | |
| POH (d) (median, range) | 9 (6-74) | 9 (6-73) | 0.75 | 14 (7-159) | 19 (10-145) | 0.1 | |
On the other hand, in the OTG group, although operative time and estimated blood loss were comparable between non-OW and OW patients, the number of retrieved lymph nodes was less (P = 0.03), local complication rate was higher (P = 0.03) and anastomotic leakage was more frequent in OW patients (P = 0.03).
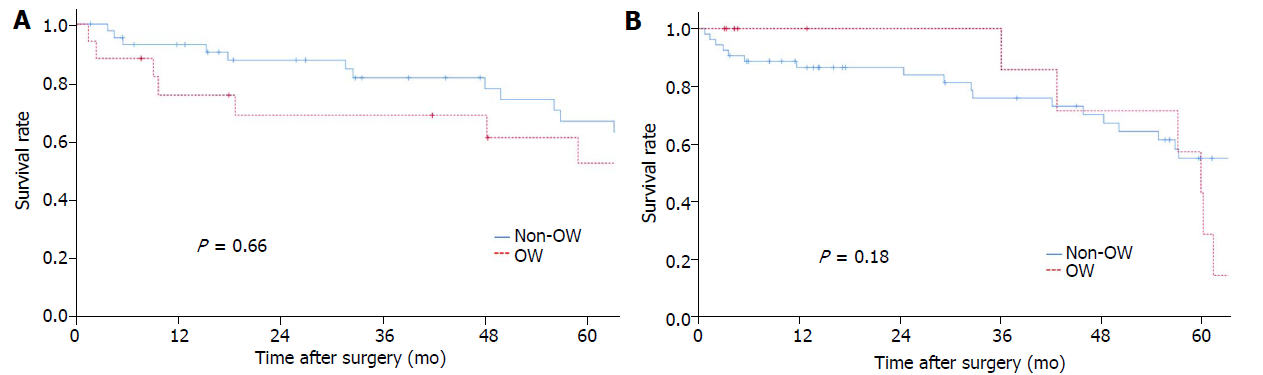
The Kaplan-Meyer curves were depicted using log-rank tests in Figure 2. The mean follow-up period was 56 mo (range, 1-156 mo). In the LTG (Figure 2A) and OTG (Figure 2B) groups, there was no survival difference between non-OW and OW patients (P = 0.66 and 0.18, respectively).
In the present study, median operative time was significantly longer, but morbidity rates were similar in OW patients than in non-OW patients in the LTG group. OS was also comparable between OW and non-OW patients in the LTG group.
OW and total gastrectomy are the factors that make surgeons reluctant to choose the laparoscopic approach due to technical difficulty. Both major drawbacks were addressed in the present study. The feasibility and safety of the laparoscopic approach in OW patients and cases of total gastrectomy were already reported[9-11,16-18], but an assessment of the feasibility and safety of LTG in OW patients has not yet been conducted.
Some articles reported the feasibility of laparoscopic distal gastrectomy in OW patients[9-11]. The present results add further evidence of the feasibility and safety of LTG in OW patients, although operative time was longer than that in non-OW patients.
Another implication of the present study’s findings is that OW might have a lesser impact in LTG than in OTG. The reasons for this are intriguing. In laparoscopic surgery, a meticulous procedure can be performed through a magnified view. Pneumoperitoneum might be another factor that can contribute to less blood loss from the adipose tissue and small vessels.
Shimada et al[9] reported that the long-term outcomes of OW patients were worse after laparoscopic distal gastrectomy and discussed that restricted lymph node dissection might be the cause. In the present study, long-term outcomes were comparable between OW and non-OW patients in the LTG group. The numbers of retrieved lymph nodes were comparable between OW and non-OW patients in the LTG group, so this might be the reason for minimizing the stage migration and also the curative effect of lymph node dissection in the present study. On the other hand, the number of retrieved lymph nodes was less in OW patients in the OTG group. Although there was no difference in the OS between OW and non-OW patients, it was implied that OW might have a greater impact for lymph node dissection in open approach.
There are two limitations of the present study. First, it was a retrospective study although the dataset was prospectively collected. Second, the number of cases was not large enough for conclusive results because propensity score matching was conducted to balance the baseline characteristics of the LTG and the OTG groups in the present study.
In conclusion, LTG in OW patients remains technically challenging but can be performed safely. Our findings also imply that OW had a lesser effect on LTG than OTG.
While the proportion of gastric cancer in upper third stomach is increasing, increased number of overweight (OW) patients is an important health issue. Consequently, laparoscopic total gastrectomy (LTG) to OW patients is increasing.
Total gastrectomy and OW seems among the worst combinations for the laparoscopic approach. However, whether OW really has a worse impact on LTG compared to open total gastrectomy remains unknown.
The main objectives of this retrospective study were to investigate safety and oncological feasibility of LTG in OW patients.
Propensity score matching selected 152 patients (76 laparoscopic, 76 open), from 321 patients who underwent total gastrectomy from 1999 to 2016. The patients were subsequently divided into the OW (≥ 25) or non-OW (< 25) group by body mass index. Postoperative outcomes of laparoscopic versus open approaches were compared between OW and non-OW groups.
In the laparoscopy group, operative time was longer (P = 0.01) in the OW group, however, other perioperative results were comparable between the non-OW and OW groups. In the open group, number of retrieved lymph nodes were less (P = 0.03) and local complication rate was more frequent (P = 0.03) in the OW group.
LTG in OW patients remains technically challenging but can be performed safely. Our findings imply that OW has a lesser effect on the laparoscopic versus open approach to total gastrectomy.
Laparoscopic approach can be a choice for total gastrectomy in OW patients in experienced institutions.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Kim BS, Li Z S- Editor: Ji FF L- Editor: A E- Editor: Wu YXJ
| 1. | Blot WJ, Devesa SS, Kneller RW, Fraumeni JF Jr. Rising incidence of adenocarcinoma of the esophagus and gastric cardia. JAMA. 1991;265:1287-1289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1287] [Cited by in RCA: 1149] [Article Influence: 33.8] [Reference Citation Analysis (0)] |
| 2. | Ahn HS, Lee HJ, Yoo MW, Jeong SH, Park DJ, Kim HH, Kim WH, Lee KU, Yang HK. Changes in clinicopathological features and survival after gastrectomy for gastric cancer over a 20-year period. Br J Surg. 2011;98:255-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 163] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 3. | Son SY, Shin DJ, Park YS, Oo AM, Jung DH, Lee CM, Ahn SH, Park DJ, Kim HH. Spleen-preserving lymphadenectomy versus splenectomy in laparoscopic total gastrectomy for advanced gastric cancer. Surg Oncol. 2017;26:207-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 4. | Kawamura Y, Satoh S, Suda K, Ishida Y, Kanaya S, Uyama I. Critical factors that influence the early outcome of laparoscopic total gastrectomy. Gastric Cancer. 2015;18:662-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 5. | Kubo M, Sano T, Fukagawa T, Katai H, Sasako M. Increasing body mass index in Japanese patients with gastric cancer. Gastric Cancer. 2005;8:39-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Bickenbach KA, Denton B, Gonen M, Brennan MF, Coit DG, Strong VE. Impact of obesity on perioperative complications and long-term survival of patients with gastric cancer. Ann Surg Oncol. 2013;20:780-787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 98] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 7. | Tokunaga M, Hiki N, Fukunaga T, Ogura T, Miyata S, Yamaguchi T. Effect of individual fat areas on early surgical outcomes after open gastrectomy for gastric cancer. Br J Surg. 2009;96:496-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 76] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 8. | Kunisaki C, Makino H, Takagawa R, Sato K, Kawamata M, Kanazawa A, Yamamoto N, Nagano Y, Fujii S, Ono HA. Predictive factors for surgical complications of laparoscopy-assisted distal gastrectomy for gastric cancer. Surg Endosc. 2009;23:2085-2093. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 94] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 9. | Shimada S, Sawada N, Ishiyama Y, Nakahara K, Maeda C, Mukai S, Hidaka E, Ishida F, Kudo SE. Impact of obesity on short- and long-term outcomes of laparoscopy assisted distal gastrectomy for gastric cancer. Surg Endosc. 2018;32:358-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 10. | Sugimoto M, Kinoshita T, Shibasaki H, Kato Y, Gotohda N, Takahashi S, Konishi M. Short-term outcome of total laparoscopic distal gastrectomy for overweight and obese patients with gastric cancer. Surg Endosc. 2013;27:4291-4296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 38] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 11. | Yamada H, Kojima K, Inokuchi M, Kawano T, Sugihara K. Effect of obesity on technical feasibility and postoperative outcomes of laparoscopy-assisted distal gastrectomy--comparison with open distal gastrectomy. J Gastrointest Surg. 2008;12:997-1004. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 67] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 12. | Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer. 2011;14:113-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1723] [Cited by in RCA: 1892] [Article Influence: 135.1] [Reference Citation Analysis (0)] |
| 13. | Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017;20:1-19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1575] [Cited by in RCA: 1903] [Article Influence: 237.9] [Reference Citation Analysis (1)] |
| 14. | Okuno K, Gokita K, Tanioka T, Ogawa N, Otsuki S, Inokuchi M, Takayama T, Kojima K. Esophagojejunostomy Using the Purse-String Suturing Device After Laparoscopic Total or Proximal Gastrectomy for Gastric Cancer. World J Surg. 2017;41:2605-2610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18532] [Cited by in RCA: 24527] [Article Influence: 1168.0] [Reference Citation Analysis (0)] |
| 16. | Lin JX, Lin JL, Zheng CH, Li P, Xie JW, Wang JB, Lu J, Chen QY, Cao LL, Lin M. Short- and long-term outcomes of laparoscopy-assisted versus open total gastrectomy for gastric cancer: a propensity score-matched analysis. Oncotarget. 2017;8:80029-80038. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 17. | Chen XZ, Wang SY, Wang YS, Jiang ZH, Zhang WH, Liu K, Yang K, Chen XL, Zhao LY, Qiu M. Comparisons of short-term and survival outcomes of laparoscopy-assisted versus open total gastrectomy for gastric cancer patients. Oncotarget. 2017;8:52366-52380. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Chen K, Xu XW, Zhang RC, Pan Y, Wu D, Mou YP. Systematic review and meta-analysis of laparoscopy-assisted and open total gastrectomy for gastric cancer. World J Gastroenterol. 2013;19:5365-5376. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 59] [Cited by in RCA: 67] [Article Influence: 5.6] [Reference Citation Analysis (0)] |